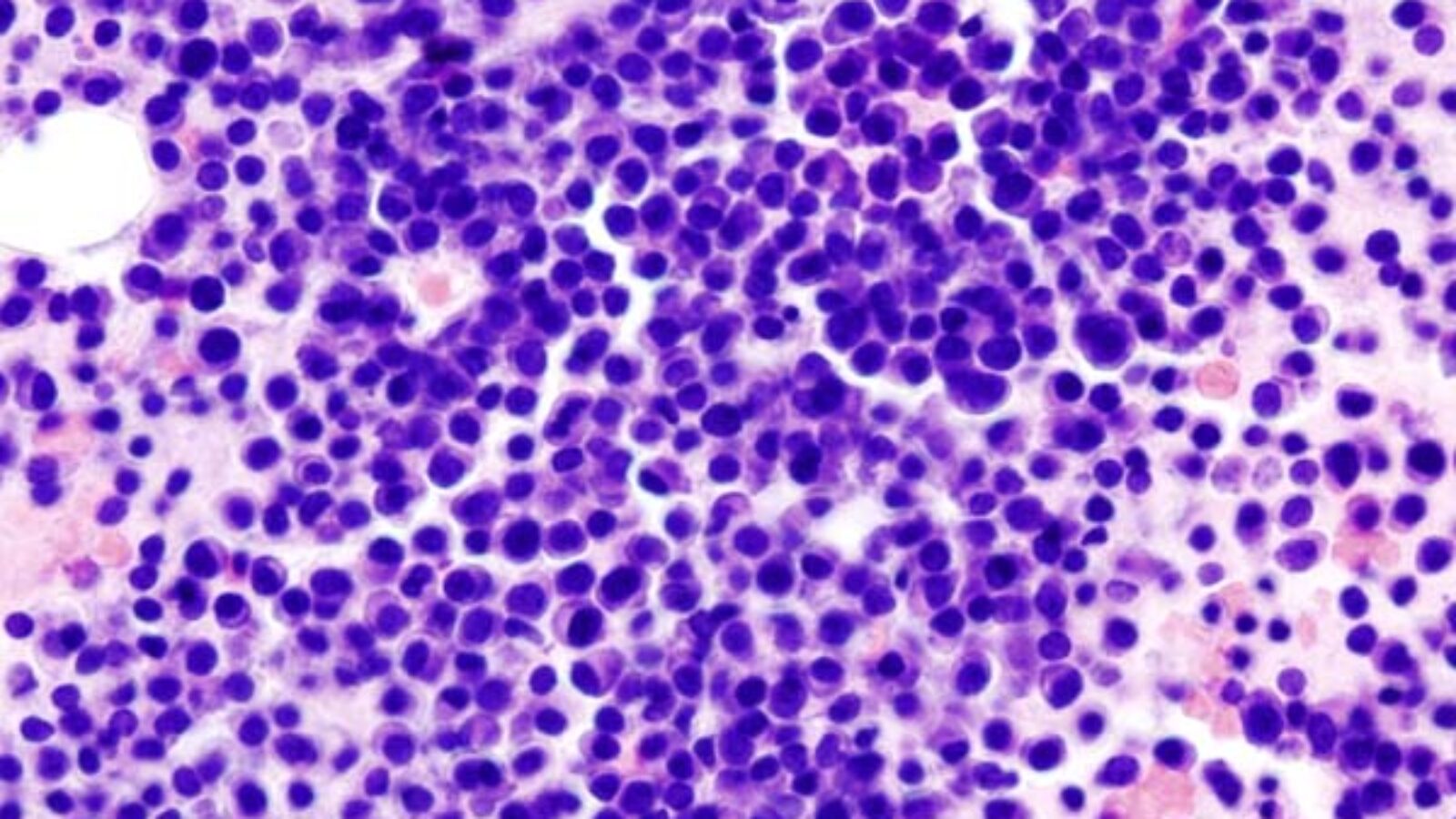
This research collaboration focuses on multiple myeloma, the most frequent tumour in bones and bone marrow, and the mechanisms behind its resistance to current immunotherapy approaches. The advent of chimeric-antigen receptor T cells (CART) targeting B cell maturation antigen (BCMA) – Idecel and Ciltacel – has significantly improved the therapy of patients with multiple myeloma. However, a considerable proportion of patients relapse within the first 12 months after treatment and have a poor prognosis. Whereas target antigen loss has been described as one reason for relapse after CART therapy in B-cell lymphoma and acute lymphoblastic leukaemia, this mode of resistance seems to be infrequent in multiple myeloma. Newer research points to tumour intrinsic factors being able to turn down the anti-myeloma immune response over time.
In a systematic screen, the team of Reuben Benjamin, King’s, has identified potential molecules and pathways which may help predict the response or resistance of individual patients. This is where the joint transCampus project starts: The group undertakes a comprehensive analysis of tumour intrinsic and tumour microenvironmental factors that mediate resistance to anti-BCMA CART cells. Therefore, a pilot study led by Raphael Teipel, University Hospital Dresden, will be carried out with samples from up to 10 relapsed myeloma patients treated with Idecel or Ciltacel. Single cell RNA seq of selected myeloma cells will be performed and bioinformatics analysis used to identify genes that correlate with depth and duration of remission achieved with CART therapy and with relapse. Separately, deep immune profiling will be performed to investigate any correlation between specific immune cell subsets and response to CART therapy.